Writer: Alisha G C
Summary
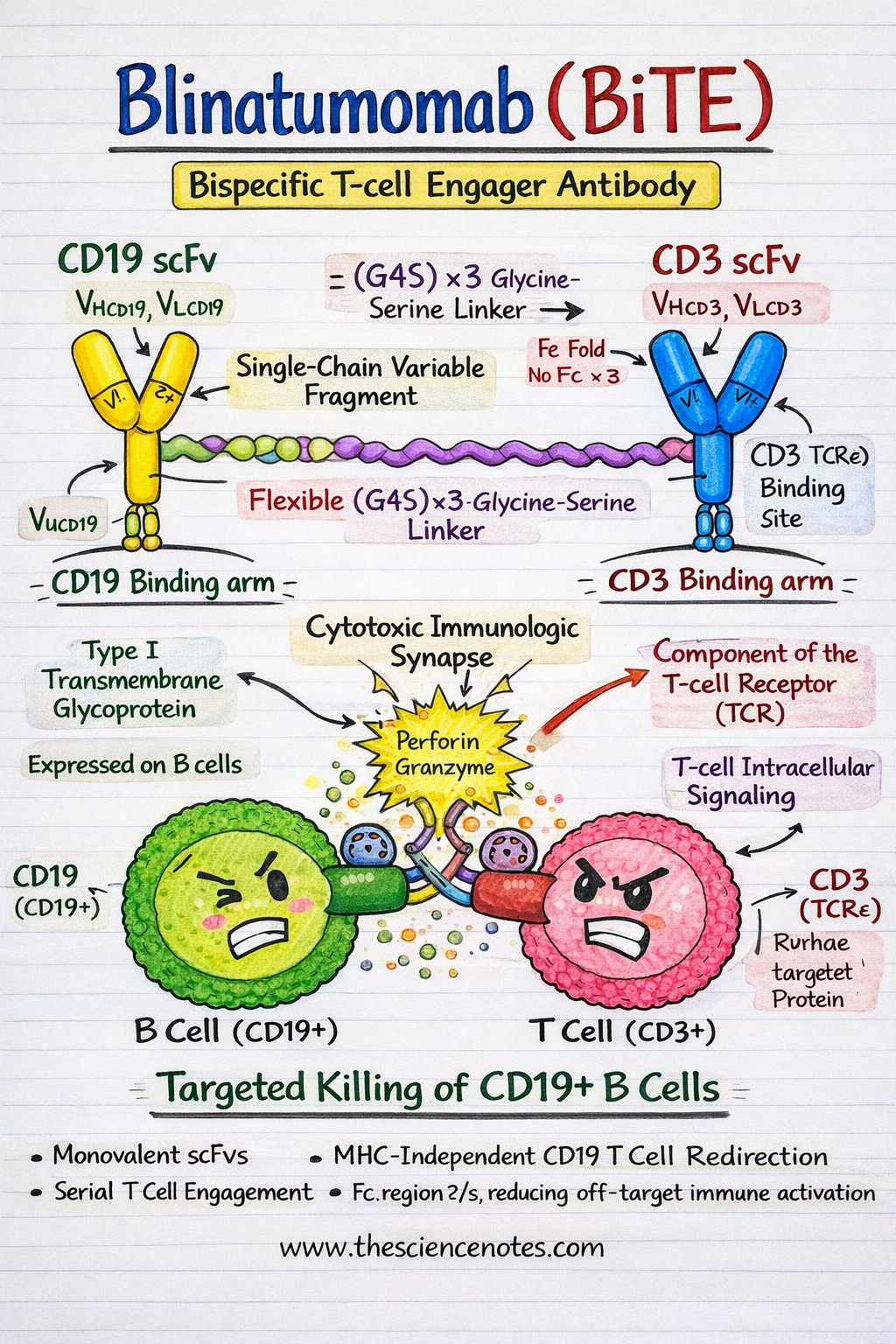
Blinatumomab is a first-in-class bispecific T-cell engager (BiTE) antibody that has essentially reshaped the therapeutic panorama of relapsed or refractory B-cell acute lymphoblastic leukemia (B-ALL). By bodily linking endogenous cytotoxic T cells to CD19-expressing malignant B cells, Blinatumomab allows potent, main histocompatibility advanced (MHC)–unbiased T-cell cytotoxicity, thereby overcoming important limitations of standard chemotherapy and antigen presentation–dependent immunotherapies. Regardless of spectacular scientific efficacy, significantly in minimal residual illness (MRD)–optimistic and closely pretreated sufferers, therapeutic resistance and illness relapse stay vital obstacles to sturdy remission. This complete evaluation gives an in-depth evaluation of Blinatumomab’s molecular structure, immunologic mechanism of motion, pharmacokinetics, scientific outcomes, resistance pathways, and rising methods to beat therapeutic failure, integrating insights from structural biology, immunology, and translational analysis.
Molecular Construction of Blinatumomab
Blinatumomab is a recombinant fusion protein composed of two single-chain variable fragments (scFvs) derived from monoclonal antibodies focusing on CD19 and CD3ε, respectively. In contrast to standard monoclonal antibodies, BiTE molecules are compact, versatile, and engineered to deliver immune effector cells into direct contact with tumor cells.
CD19 scFv: The B-Cell Concentrating on Area
CD19 is a 95 kDa sort I transmembrane glycoprotein belonging to the immunoglobulin superfamily and is expressed all through most levels of B-cell growth, from pre-B cells to mature B lymphocytes. Functionally, CD19 acts as a coreceptor of the B-cell receptor (BCR) advanced, the place it amplifies signaling by reducing activation thresholds and regulating downstream pathways comparable to PI3K–AKT and SYK signaling.
From a therapeutic perspective, CD19 is a perfect immunotherapy goal resulting from:
-
Expression in >95% of B-ALL circumstances
-
Secure floor localization throughout leukemogenesis
-
Minimal expression exterior the B-cell lineage, lowering off-target toxicity
The CD19 scFv in Blinatumomab acknowledges an extracellular epitope that continues to be accessible even in low-antigen–density states, enabling environment friendly engagement of malignant B cells.
CD3ε scFv: The T-Cell Engagement Area
CD3ε is a vital signaling part of the T-cell receptor (TCR) advanced, related to CD3γ, CD3δ, and the CD3ζ homodimer. Upon engagement, CD3ε transduces activation indicators via immunoreceptor tyrosine-based activation motifs (ITAMs) current on CD3ζ chains.
Importantly, Blinatumomab binds CD3ε independently of antigen specificity, permitting recruitment of polyclonal, non–tumor-specific T cells. This mechanism bypasses the necessity for peptide antigen processing and presentation, a frequent immune-evasion technique in leukemia.
Linker Design and Structural Configuration
The 2 scFvs are related through a versatile, non-immunogenic (Gly₄Ser)₃ linker, producing a ~55 kDa BiTE molecule. This linker gives enough rotational freedom to permit simultaneous binding of CD19 and CD3 with out steric hindrance.
A defining function of Blinatumomab is the absence of an Fc area, which:
-
Enhances tissue penetration and diffusion
-
Eliminates Fcγ receptor binding
-
Reduces off-target immune activation, together with ADCC and CDC
-
Minimizes nonspecific cytokine launch
Key Structural Options
-
Monovalent scFv binding allows fast serial engagement of a number of tumor cells
-
Versatile linker structure helps secure immunologic synapse formation
-
Quick serum half-life (~2 hours) permits exact pharmacokinetic management through steady IV infusion
-
Fc-less design improves security and specificity
Crystallographic and biophysical research affirm that the spatial orientation of the CD19 and CD3 binding arms is perfect for intercellular tethering, leading to environment friendly formation of a practical cytolytic immunologic synapse.
Mechanism of Motion of Blinatumomab
1. Immunologic Synapse Formation and T-Cell Redirection
Blinatumomab mediates MHC-independent T-cell cytotoxicity by bodily bridging CD3+ T cells and CD19+ leukemic B cells, successfully changing resting T cells into serial tumor killers.
-
Bipartite engagement induces TCR clustering via CD3ε whereas anchoring malignant B cells through CD19
-
This pressured proximity mimics physiological immune synapse formation
On the synapse, key signaling molecules comparable to Lck, LAT, SLP-76, PKCθ, and actin-regulatory proteins are recruited and spatially organized.
Intracellular Sign Transduction
Upon CD3 engagement:
-
Lck phosphorylates ITAMs on CD3ζ chains
-
ZAP-70 is recruited and activated
-
Adaptor proteins (LAT, SLP-76) assemble signaling complexes
-
Calcium inflow and diacylglycerol (DAG) manufacturing activate:
-
Calcineurin → NFAT
-
PKCθ → NF-κB
-
MAPK cascade → AP-1
-
These transcriptional packages drive T-cell activation, proliferation, and cytotoxic perform.
Effector Features
-
Perforin–granzyme B–mediated apoptosis
-
Launch of pro-inflammatory cytokines (IFN-γ, IL-2, TNF-α)
-
Serial killing, the place a single T cell disengages and targets a number of leukemic cells
2. T-Cell Reprogramming and Immune Reminiscence
Past fast cytotoxicity, Blinatumomab induces practical reprogramming of T cells, selling growth of:
These populations contribute to long-term immune surveillance and should underlie sustained MRD negativity noticed in responding sufferers.
3. Pharmacokinetics and Immune Dynamics
Resulting from its small dimension and lack of Fc area, Blinatumomab displays:
-
Fast clearance through renal filtration and proteolysis
-
Peak T-cell activation and growth between days 7–14
-
Preferential growth of CD8+ cytotoxic T cells, correlating with depth of response
Steady intravenous infusion ensures secure plasma concentrations whereas permitting fast cessation within the occasion of toxicity.
Scientific Efficacy of Blinatumomab in B-ALL
TOWER Trial (NEJM, 2017)
-
Grownup relapsed/refractory B-ALL
-
CR/CRh: 43% vs 25% (Blinatumomab vs chemotherapy)
-
Median total survival: 7.7 vs 4.0 months
BLAST Trial (Blood, 2018)
-
MRD-positive B-ALL in hematologic remission
-
MRD clearance: 78% after one cycle
-
3-year total survival: 71%
Hostile Occasions
-
Cytokine launch syndrome (CRS): early onset, sometimes steroid-responsive
-
Neurotoxicity: grade ≥3 in ~10%, probably linked to T-cell trafficking throughout the blood–mind barrier
Mechanisms of Resistance to Blinatumomab
1. Antigen Escape (CD19 Loss)
-
Different splicing (e.g., exon 2 skipping)
-
CD19 gene mutations or deletions
-
Lineage change to myeloid phenotype, significantly in MLL-rearranged leukemia
2. T-Cell Intrinsic Resistance
-
Upregulation of exhaustion markers (PD-1, TIM-3, LAG-3)
-
TOX-dependent epigenetic reprogramming
-
Metabolic insufficiency and mitochondrial dysfunction
3. Immune Checkpoint and Microenvironmental Suppression
-
PD-L1 upregulation on leukemic blasts and MDSCs
-
Immunosuppressive cytokines (IL-10, TGF-β)
-
Growth of regulatory T cells and suppressive monocytes
Methods to Overcome Blinatumomab Resistance
Twin and Multispecific Concentrating on
Checkpoint Inhibition
T-Cell Health Enhancement
Subsequent-Technology BiTE Platforms
Conclusion
Blinatumomab represents a paradigm shift in B-ALL immunotherapy, enabling exact, MHC-independent T-cell redirection with substantial scientific profit throughout a number of illness settings. Whereas resistance mechanisms comparable to antigen escape, T-cell dysfunction, and immune suppression stay vital obstacles, rational mixture therapies, next-generation BiTE engineering, and immune profiling–guided methods supply promising avenues to reinforce sturdiness of response. Continued integration of molecular biology, immunology, and scientific innovation can be important to increasing the therapeutic window of Blinatumomab and reaching long-term cures in B-ALL.
Often Requested Questions (FAQ)
Q1. What’s Blinatumomab and the way does it work?
Blinatumomab is a bispecific T-cell engager (BiTE) antibody that hyperlinks CD3-positive T cells to CD19-positive B cells, triggering MHC-independent T-cell–mediated cytotoxicity.
Q2. Why is CD19 a really perfect goal in B-ALL?
CD19 is expressed in over 95% of B-cell acute lymphoblastic leukemia circumstances and is absent from most non–B-lineage tissues, minimizing off-target toxicity.
Q3. What are the primary resistance mechanisms to Blinatumomab?
Resistance arises from CD19 antigen loss, T-cell exhaustion, immune checkpoint upregulation, and suppressive tumor microenvironment components.
This autumn. How does Blinatumomab differ from CAR-T cell remedy?
In contrast to CAR-T remedy, Blinatumomab redirects endogenous T cells with out genetic modification and permits exact pharmacokinetic management via steady infusion.
Q5. What are rising methods to beat Blinatumomab resistance?
Approaches embrace dual-target BiTEs, checkpoint inhibitor mixtures, cytokine-based T-cell assist, and next-generation trispecific engager platforms.

